Vitamin D deficiency has consequences well beyond bone health.
Vitamin D is gold.
Vitamin D is so important to the body, immune cells, brain, colon, breast, and other cells have the ability to also activate it locally when required. Although labelled a vitamin, calcitriol (bio-active vitamin D) acts more like a hormone within the body. It is involved in many essential functions well beyond bone health. Vitamin D is critical for inflammatory modulation, hormonal and immune functions as well as cardiovascular, mental health and pancreatic function. The active form of vitamin D interacts with receptors in the intestine, bone, brain, heart, immune cells and skeletal muscle. Vitamin D functions as a modulator of up to 1000 genes involved in cellular growth and protein synthesis.
Vitamin D plays an important role in an athlete’s health, training and performance.
Studies show it may even be necessary for optimal muscle function and performance as muscle performance is impaired by suboptimal vitamin D status. Deficiency induces atrophy of fast twitch muscle fibers, impairs calcium uptake and prolongs time to peak contractile tension and relaxation. Studies also show Vitamin D deficiency may delay rehabilitation from injury.
In sporty pregnant women, low vitamin D levels are linked to pre-eclampsia, gestational diabetes and adverse pregnancy outcomes. Vitamin D also plays a part in regulating insulin, blood sugar balance and thyroid hormones. Research shows that a deficiency of vitamin D is associated with a high risk of thyroid antibodies, which are found in individuals with autoimmune thyroid disorders.
Vitamin D is most commonly known in the athletic community for its influence on bone health and prevention of bone injury. Vitamin D influences bone health by upregulating expression of genes that enhance intestinal calcium absorption, and reabsorption by the kidneys along with increasing bone-building cell activity. Studies show calcium absorption significantly increases when vitamin D levels are sufficient. Calcium absorption is reduced to 10-15% with low vitamin D levels and stress fracture risk significantly increases.
Typically, 80% of our vitamin D is obtained from the sun and 20% from food sources.
Signs of Vitamin D deficiency
- fatigue and tiredness
- lower back pain
- recurrent colds and infections and poor immunity
- stress fractures
- heaviness in the legs
- recurrent injuries
- muscle pain, weakness, poor muscle contraction and relaxation
- mental health issues, low mood, seasonal sadness and depression
- hormonal imbalances and PMS
- anaemia and low iron
- pale floating stool
- photosensitivity
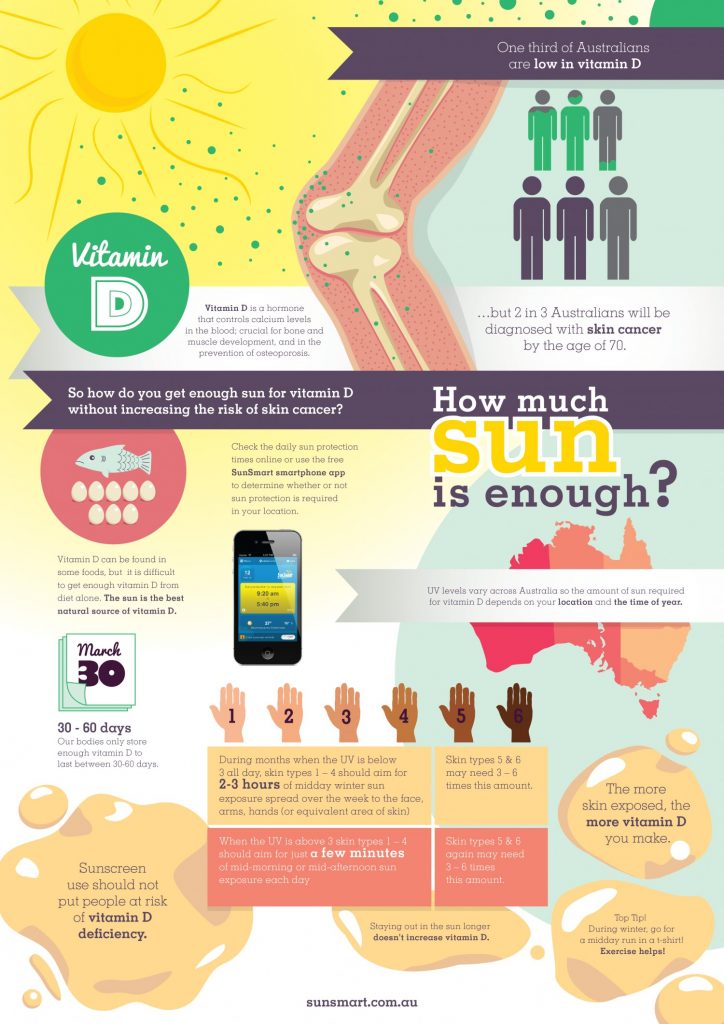
According to Sunsmart Australia, one-third of Australians are low in Vitamin D.
 10 Reasons your vitamin D is low
10 Reasons your vitamin D is low
Vitamin D can be made by our body when skin is exposed to sunlight through a complex activation process, however, what many people fail to realise is that this process doesn’t always occur efficiently or reach levels required for optimal health. Vitamin D production may vary depending on the time of day of sun exposure, season, cloud cover, smog, latitude, skin pigmentation, age, and sunscreen use.
We often see patients with low levels of vitamin D despite being out in the sun daily. There are several reasons why vitamin D levels drop despite sunlight exposure.
1. As vitamin D is fat-soluble and stored in fat cells, individuals with low body fat, may be disposed to vitamin D deficiency as their storage tank is smaller.
2. Activation and production of vitamin D are inhibited by magnesium deficiency, inflammation, and excessive use of sunscreen.
3. Individuals with any form of malabsorption issues, liver or kidney issues, coeliac’s disease, Crohn’s, vegans, and thyroid issues can be prone to deficiencies.
4. Anyone with a history of anaemia should also be aware of the bidirectional influence between iron and vitamin D. The activation of vitamin D in the kidneys requires iron-containing compounds ferredoxin reductase and ferredoxin. Iron deficiency may therefore contribute to the inactivation of vitamin D. Vitamin D deficiency may also be associated with higher hepcidin (a pro-inflammatory mediator) in the liver. Hepcidin will elevate ferritin stores and down-regulate intestinal absorption of iron from food and impair storage iron release. Hundreds of athletes have used our handy anaemia tool to help determine the likely risk of having low iron or anaemia.
5. Diets containing limited seafood, eggs or dairy such as vegan diets may also reduce vitamin D intake.
6. Insufficient direct UVB exposure (due to smog, cloud cover or latitude), early- or late-day training, indoor training, geographic location further away from the equator and sunscreen use (SPF of 15 lowers vitamin D synthesis capacity by 98%).
7. Disruption to the microbiota and gut inflammation may also affect the availability of vitamin D.
8. In addition some individuals may find it difficult to increase their vitamin D levels if they have low antioxidant status.
9. Medications such as anticonvulsants, corticosteroids, cimetidine, theophylline, statins or the weight loss drug orlistat.
PATHOLOGY TESTING
As a general guide, Osteoporosis Australia recommends most people should have levels of at least 50 nmol/L at the end of winter, which means people may have higher levels during summer (60-70 nmol/L). However, in order to maintain optimal health, athletes should aim for serum levels over 90 nmol/L ideally between 100 and 130 nmol/L.
Treatment
Daily sunlight exposure on your skin especially on large areas such as the back, chest, legs and arms (25-60 minutes in winter) without suntan cream, is a great way to keep levels topped up. Athletes living in southern states of Australia and New Zealand need 30 minutes of direct skin exposure (springtime) on large areas of skin such as back, arms, chest or legs closer to midday. Athletes living closer to the equator may require 15 minutes before 10 am. During this time avoid putting sunscreen on, then for the rest of the day, cover up. Lunchtime exercise with as much skin exposure as possible (within decency) is a great way to give yourself a vitamin D fix, especially in winter months.
Get tested biannually- before winter and again in spring.
Consume vitamin D-rich foods on a daily basis such as oily fish like cod, salmon, sardines or tuna, egg yolks, sun-dried mushrooms, and fortified milk, butter and fortified cereals. Some individuals may benefit from cod liver oil which also contains vitamin A and essential fatty acids.
When levels are low, take a quality supplement in the correct dosage range and a probiotic. Certain probiotics such as Lactobacillus rhamnosus LGG and Lactobacillus plantarum enhance levels synergistically.
Obtain adequate magnesium-rich foods such as spinach, pumpkin seeds, almonds, black beans, oyster mushrooms, avocado, figs, yogurt or kefir and banana. Chocolate also contains magnesium.
About the Author: Kate Smyth is a Sports naturopath, nutritionist and female-centric running coach. She is the founder of the Athlete Sanctuary- a holistic healthcare clinic for athletes of all levels and sporting codes. Kate has a thirst for knowledge with two bachelor’s and a master’s degree under her belt. She has been involved in sports for many decades and competed for Australia in the Commonwealth Games and Olympic Games marathons with a personal best time of 2 hours 28 minutes. For more information visit www.athletesanctuary.com.au



